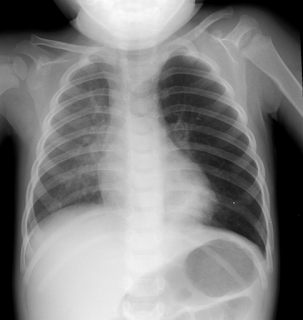
Pediatric X ray urologists, radiologists team up to devise standard protocol for VCUGs
To improve patient
safety and standardize data obtained from a voiding cystourethrogram (VCUG),
the AAP Section on Radiology and Section on Urology have established a standard
protocol for performing the test.
Establishing a
Standard Protocol for the Voiding Cystourethrography, a new clinical report, is
available at http://dx.doi.org/10.1542/peds.2016-2590 and will be published in
the November issue of pediatric x ray.
Need for standard protocols
Pediatric urologists
base many of their treatment plans and diagnoses on images obtained by their
local radiology department. Protocols ensure that the same region of the body
is imaged with the same technique each time to allow observation of disease,
set surgical indications or judge postoperative results. Standard protocols
play an important role in comparing results among institutions and facilitate
multicenter studies. Therefore, most imaging studies are required to be
performed according to national, and often international, agreed-upon protocols
to compare results and ensure patient safety.
In 2014, a standard
protocol was formulated by the American College of Radiology and the Society
for Pediatric Radiology in their practice parameters for the performance of the
VCUG. However, in practice, VCUG protocols differ significantly among institutions.
Impact of differences
A survey of 65
pediatric radiology chairs at national children's hospitals demonstrated that
the VCUG protocols are very different throughout the U.S. and Canada.
Statistically significant differences were reported concerning the amount of
bladder filling, whether immobilization and sedation were used, the formula by
which to predict bladder capacity and the height of contrast above the patient.
Differences in individual test parameters can have a significant effect on the
outcome of the test and have the potential to influence management protocols of
individual patients.
In a study on 183
patients after Deflux injection (substance injected around the opening of one
or both ureters to prevent urinary reflux), 60% of patients with a
postoperative positive VCUG result did not show vesicoureteral reflux (VUR)
until the bladder was filled over the age-adjusted bladder capacity. If an
alternative protocol had been used that filled the bladder just to the
age-adjusted capacity, those patients would have had a negative VCUG, and their
surgery would have been labeled successful. Therefore, the postoperative
success rates would be a function not only of the surgical technique and skill
of the surgeon but also of the specific VCUG imaging technique.
Recent AAP
guidelines recommend a VCUG for children between 2 and 24 months of age under
certain conditions such as after recurrence of a febrile urinary tract
infection, but they do not specify how this test should be performed (Urinary
Tract Infection: Clinical Practice Guideline for the Diagnosis and Management
of the Initial UTI in Febrile Infants and Children 2 to 24 Months,
http://bit.ly/2cZTbx4).
Different VCUG
protocols undoubtedly impact the detection and grade of VUR but also may have a
direct effect on the reporting of postoperative results. The complexity of the
VCUG makes it difficult to compare two protocols that are different in several
aspects of the test.
All of these factors
prompted a consensus group of pediatric urologists and radiologists to
formulate a standard protocol (see box) for the VCUG to be recognized and
followed by both societies. The protocol serves as guidance for the clinician
in rendering pediatric care.
Template for voiding
cystourethrogram
Patient name; date
of birth; medications; medical record number;
Date of study:
Reason for
examination: Information provided by ordering physician
Comparison: Previous
studies
Technique:
Informed consent is
obtained and documented in the patient’s record.
1. Observe ALARA (As
Low As Reasonably Achievable for minimizing radiation exposure) and Image
Gently principles.
2. Observe
recommendations for possible sedation.
3. Observe
recommendations for possible immobilization.
4. Toilet trained:
Allow patient to void in private bathroom immediately before the study.
5. After voiding and
for non-toilet-trained individuals: Insert a small age-appropriate (3.5-8
French) nonballoon catheter using sterile technique.
6. Measure postvoid
residual (PVR) urine in mL.
7. Obtain a single
anterior-posterior (AP) scout image covering the kidneys, ureters and bladder.
8. Retrograde fill
the bladder (bladder filling) with radiographic contrast at body temperature.
9. During filling,
obtain multiple spot images in AP, right and left oblique, and lateral
position.
10. Fill bladder
until voiding occurs and stop contrast flow.
11. Obtain voiding
images of the urethra.
12. Refill bladder until voiding occurs.
13. Obtain voiding
and postvoid images of the kidneys and bladder.
14. Reord maximum
amount of contrast instilled.
Dr. Frimberger, a
lead author of the
pediatric clinical report, is a Section Affiliate member of the AAP
Section on Urology.



Comments
Post a Comment